Introduction to Basal Cell Skin Cancer
Basal cell skin cancer is the most frequently diagnosed type of skin cancer, particularly prevalent among older adults. It is a form of non-melanoma skin cancer that originates in the basal cells—small, round cells found in the lower part of the epidermis. Understanding its early signs and potential locations of growth is vital for early detection and treatment, which can significantly improve outcomes and reduce complications.
This type of cancer is primarily caused by prolonged exposure to ultraviolet (UV) radiation from the sun or tanning beds, making it more common in individuals with fair skin who have a history of sunburns or excessive sun exposure. Despite its prevalence, basal cell skin cancer is considered less aggressive compared to other skin cancers, such as melanoma, because it rarely spreads to other parts of the body. However, if left untreated, it can cause significant damage to the surrounding tissues and lead to disfigurement.
In this article, we will explore the early signs of basal cell skin cancer, discuss common areas where it tends to grow, and delve into the latest treatment innovations that offer hope for effective management. By increasing awareness and understanding, individuals can take proactive steps towards prevention and early intervention.
Recognizing Early Signs of Basal Cell Skin Cancer
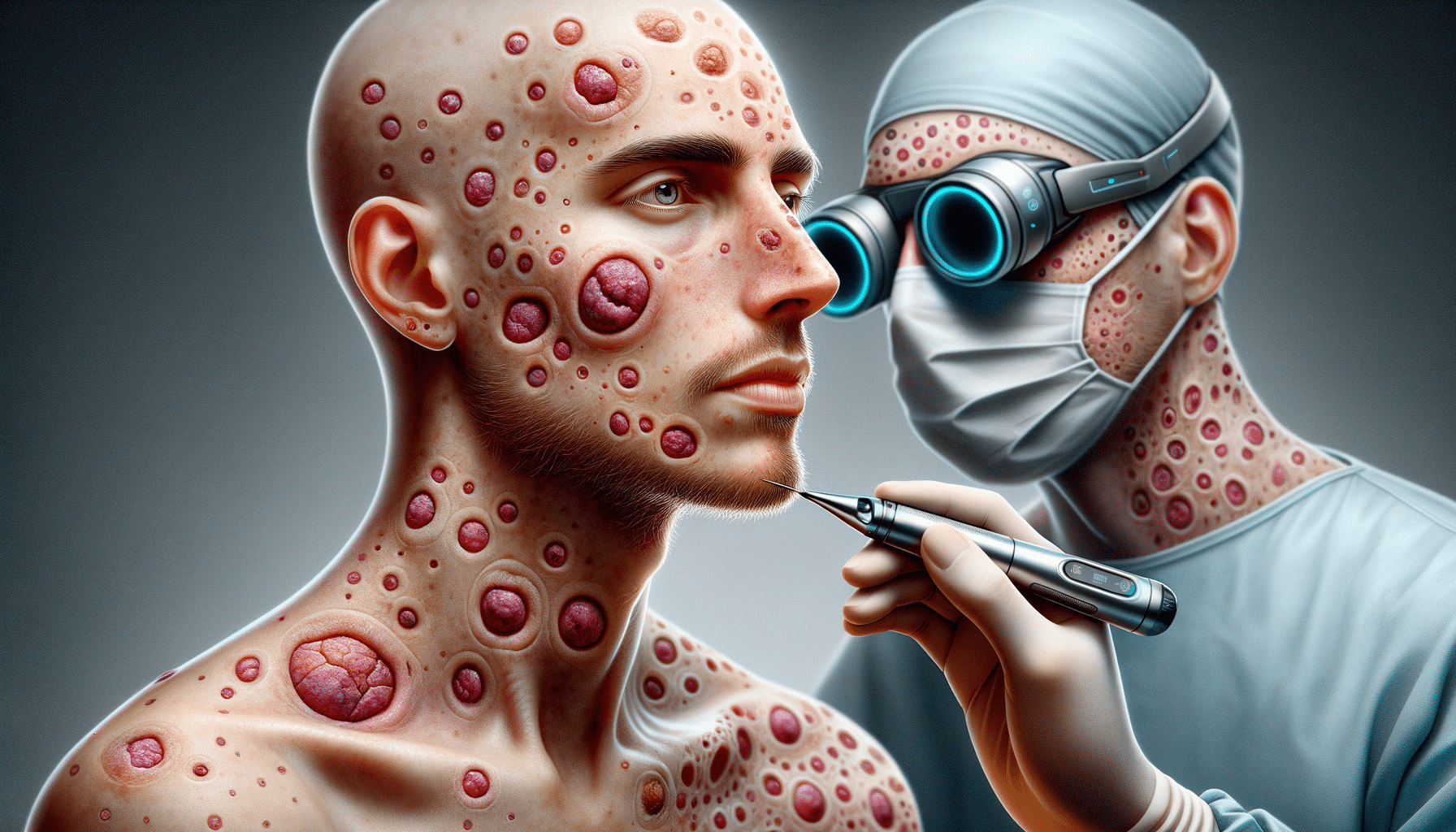
Identifying basal cell skin cancer in its early stages is crucial for successful treatment. The cancer often presents itself as a small, pearly bump or a flesh-colored mole-like growth on the skin. These lesions typically appear on sun-exposed areas, such as the face, neck, and arms. In some cases, the cancer may manifest as a flat, scaly patch or a sore that does not heal, which can be mistaken for a persistent pimple or blemish.
Key indicators to watch for include:
- A shiny, translucent bump with visible blood vessels.
- A flat lesion with a scaly, crusted surface.
- A white, waxy scar-like lesion without a clear border.
- A sore that bleeds, oozes, or crusts and remains open for weeks.
These symptoms may vary depending on the individual and the specific type of basal cell carcinoma. It is essential to consult a healthcare professional if any suspicious changes in the skin are observed. Early detection through regular skin examinations and self-checks can lead to prompt treatment and a higher likelihood of a positive outcome.
Common Growth Locations of Basal Cell Skin Cancer
Basal cell skin cancer primarily develops on areas of the skin that receive the most sun exposure. The face, ears, neck, scalp, shoulders, and back are the most common sites for these cancers to appear. The face, in particular, is a frequent location, with lesions often forming on the nose, cheeks, and around the eyes.
While sun-exposed areas are the most typical sites, basal cell carcinoma can also occur in less exposed regions, such as the chest and legs, especially in individuals with a history of significant sun exposure or tanning bed use. It’s important to note that the cancer can develop in any skin area, regardless of sun exposure, although this is less common.
Understanding where basal cell skin cancer is likely to grow helps in conducting thorough skin checks. Individuals should pay close attention to any new or changing lesions, particularly in areas that are frequently exposed to the sun. Regular dermatological check-ups can aid in early detection and prevent the cancer from advancing to a more severe stage.
Innovative Treatments for Basal Cell Skin Cancer
The treatment of basal cell skin cancer has evolved significantly, with numerous innovative options available that enhance patient outcomes and minimize side effects. Traditional treatments include surgical excision, where the cancerous tissue is removed, and Mohs surgery, a technique that involves excising the cancer layer by layer while preserving as much healthy tissue as possible.
Recent advancements have introduced non-surgical treatments, such as topical medications and photodynamic therapy. Topical treatments involve applying medicated creams directly to the cancerous lesions, which can be effective for superficial basal cell carcinomas. Photodynamic therapy uses a photosensitizing agent and a specific wavelength of light to destroy cancer cells, offering a non-invasive alternative with minimal scarring.
In addition to these, targeted therapies and immunotherapies are emerging as promising options for advanced cases. Targeted therapies focus on specific genetic mutations within the cancer cells, while immunotherapies enhance the body’s immune response to fight the cancer. These treatments represent a significant shift towards personalized medicine, offering hope for those with more complex or recurrent basal cell skin cancers.
Conclusion: Staying Vigilant Against Basal Cell Skin Cancer
Basal cell skin cancer, while common, is a manageable condition when detected early. Awareness of its early signs, understanding where it typically grows, and being informed about the latest treatment innovations are key to effective management. Regular skin checks and protective measures against UV exposure are crucial preventive steps.
For individuals at higher risk, such as those with fair skin or a history of sunburns, proactive monitoring and consultation with healthcare professionals can make a significant difference. By staying informed and vigilant, individuals can take control of their skin health and reduce the risk of complications associated with basal cell skin cancer.


Leave a Reply