How Are Sleep Apnea Treatments Evolving ?
Outline:
– Overview of sleep apnea: definitions, types, and impact
– Diagnostic approaches: overnight studies to at-home testing
– Established treatments: positive airway pressure, oral devices, surgeries
– Emerging therapies: nerve stimulation, positional aids, algorithms, telehealth support
– Living with treatment: adherence strategies, lifestyle, long-term outcomes, conclusion
Sleep Apnea 101: What It Is and Why It Matters
Sleep apnea is a disorder in which breathing repeatedly pauses or becomes shallow during sleep, fragmenting rest and lowering oxygen levels. The two main types are obstructive sleep apnea (OSA), caused by a collapsible upper airway, and central sleep apnea (CSA), where the brain’s drive to breathe falters. A third category, mixed or complex sleep apnea, combines features of both. Clinicians commonly quantify severity with the apnea–hypopnea index (AHI): events per hour of sleep, with typical thresholds of mild (5–14), moderate (15–29), and severe (30 or more). Although often associated with loud snoring and gasping, the truer signature is unrefreshing sleep and daytime impairment—slowed reaction time, morning headaches, and irritability.
OSA is widespread; estimates suggest hundreds of millions of adults globally carry some degree of the condition. Untreated, it has been linked to elevated risks of high blood pressure, coronary disease, irregular heart rhythms, insulin resistance, and motor vehicle crashes. Mechanistically, repeated arousals trigger sympathetic nervous system surges, momentary spikes in blood pressure, and inflammatory cascades. Intermittent dips in oxygen can stress the heart and blood vessels, while sleep fragmentation degrades memory consolidation, mood regulation, and metabolic balance. In CSA, unstable ventilatory control or medical conditions such as heart failure can lead to periodic breathing, sometimes with a waxing-and-waning pattern.
Beyond physiology, sleep apnea touches relationships and livelihoods. Bed partners endure disrupted nights; workers face foggy mornings and reduced productivity. Children may observe a parent nodding off at the dinner table; athletes notice stalled recovery. Fortunately, recognition is improving. Primary care screening is more common, employers invest in sleep wellness, and home-based testing has lowered barriers to evaluation. Still, diagnosis and follow-through remain uneven—many people normalize daytime sleepiness or attribute it to stress. A practical way forward is to treat sleep apnea like any chronic condition: identify the type, measure severity, tailor treatment, and track results. This approach, increasingly supported by technology and better-designed therapies, is changing outcomes from frustrating to manageable, night by night.
From Suspicion to Diagnosis: How We Find Sleep Apnea Today
The diagnostic journey usually starts with a clinical story: loud snoring, witnessed breathing pauses, nocturnal choking, morning dryness, or unrelenting sleepiness. Screening tools can structure that story—questionnaires that tally risk factors such as neck circumference, age, craniofacial features, and blood pressure. These instruments help prioritize who should be tested, but they do not confirm the disorder. Confirmation comes from sleep testing, either a full in-lab polysomnogram or a streamlined home sleep apnea test (HSAT) in appropriate cases.
Polysomnography is the comprehensive option, measuring brain waves, eye movements, chin and leg muscle activity, heart rhythm, airflow, respiratory effort, and oxygen saturation. It can identify OSA, CSA, and other sleep disorders such as periodic limb movements or parasomnias. Because it captures sleep stages and arousals directly, it provides nuanced data on how breathing instability fragments sleep. HSAT, by contrast, records fewer signals—typically airflow or nasal pressure, respiratory effort bands, and oxygen saturation—without direct brain-wave monitoring. It is well-suited for adults with a high likelihood of moderate-to-severe OSA and without major comorbidities that could complicate interpretation.
Who needs an in-lab study rather than HSAT? Situations often include:
– Significant heart or lung disease, opioid use, or suspected CSA
– Neuromuscular conditions or hypoventilation syndromes
– Occupations where diagnostic certainty is critical (e.g., public safety roles)
– Prior inconclusive HSAT or mismatch between symptoms and results
Results are scored to calculate indices: the AHI, oxygen desaturation burden, arousal counts, and positional patterns. Positional OSA (worse on the back) and REM-related OSA (worse in dream sleep) are common—and actionable—phenotypes. Growing interest in wearable sensors and consumer sleep trackers has broadened awareness, but these devices are not diagnostic and can both over- and underestimate events. Their most constructive role is to prompt conversation with a clinician when persistent snoring, fatigue, or morning headaches surface. Telemedicine has also transformed access; pretest counseling, equipment pickup, and follow-up discussions now often happen remotely, with data uploaded for timely interpretation. The goal is consistent: pair the right test with the right person, then transform numbers into a plan that restores restorative sleep and daytime clarity.
Established Treatments: Positive Airway Pressure, Oral Devices, and Surgery
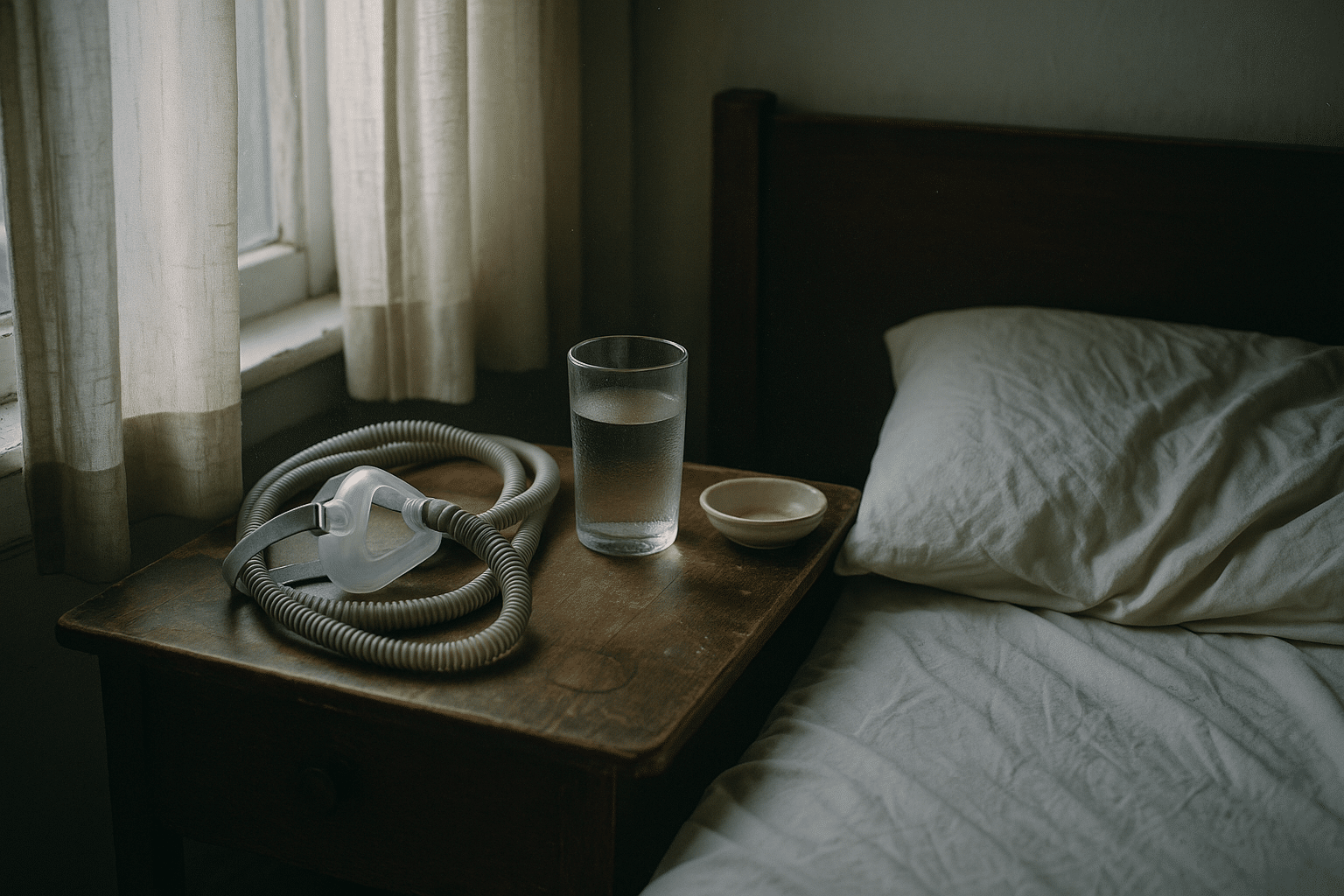
For moderate-to-severe OSA, positive airway pressure (PAP) therapy remains a cornerstone. By gently splinting the upper airway open with a column of air, PAP can normalize AHI and improve sleepiness, blood pressure, and quality of life for many users. Modes vary: fixed-pressure devices deliver one setting determined by a titration study, auto-adjusting systems vary pressure within a prescribed range, and bilevel support provides different pressures for inhale and exhale in select scenarios. Masks come in several styles—nasal pillows, nasal cushions, and full-face interfaces—each with trade-offs in seal, comfort, and mouth breathing management. Common hurdles include nasal dryness, congestion, skin irritation, and a sense of pressure; heated humidification, proper strap tension, and gradual ramp features help many patients adapt.
Mandibular advancement devices (MADs) are custom oral appliances fitted by trained dental professionals. By holding the lower jaw slightly forward, they enlarge the airway space and stiffen tissues, particularly effective in mild-to-moderate OSA or when PAP is not tolerated. Side effects can include jaw soreness, tooth discomfort, and, over time, bite changes; regular follow-up and periodic sleep testing help optimize advancement and verify efficacy. For appropriately selected patients, MADs can meaningfully reduce snoring and AHI, with adherence sometimes higher than PAP because of portability and simplicity.
Surgery targets structural contributors to airway collapse. Procedures range from nasal septal or turbinate work (improving airflow) to soft palate and tongue-base operations that reduce tissue volume or reposition anatomy. In carefully chosen cases, maxillomandibular advancement—moving both jaws forward—can yield large and durable improvements by expanding the entire airway framework. Selection relies on anatomical evaluation, sometimes aided by drug-induced sleep endoscopy to visualize collapse patterns. As with any surgery, benefits must be weighed against recovery time, potential complications, and variable response.
Choosing among established therapies involves a practical matrix:
– PAP: high physiologic efficacy when used consistently; requires acclimation and maintenance
– MADs: portable and discreet; effectiveness may be lower than PAP but adherence can be strong
– Surgery: anatomical solution for select profiles; involves procedural risk and variable outcomes
Many patients combine approaches over time—using PAP for core control, adding positional strategies, optimizing nasal airflow, or transitioning to an oral device for travel. The guiding principle is personalization: the right tool, for the right airway, at the right moment in a person’s life.
New Frontiers: Personalization, Devices, and Data-Driven Care
Sleep apnea treatment is moving toward precision: identifying which mechanism drives a person’s events and tailoring therapy accordingly. One notable development is upper airway nerve stimulation, an implantable system that senses breathing and times a gentle pulse to the nerve controlling tongue movement, keeping the airway open during inspiration. For selected adults with moderate-to-severe OSA who cannot tolerate PAP and meet specific anatomical and physiological criteria, studies report meaningful reductions in AHI and sleepiness scores along with improved daytime function. While the approach requires surgery and ongoing follow-up, it has expanded choices beyond masks and oral devices.
Non-implant options are evolving too. Positional therapy uses soft bands or small wearable trainers that encourage side sleeping, often effective for position-dependent OSA. Nasal expiratory resistance devices create a mild backpressure during exhalation, which can stabilize the airway in some people with mild disease. Myofunctional therapy—structured exercises targeting tongue, soft palate, and oropharyngeal muscles—has shown promise as an adjunct, particularly for snoring and mild OSA, though results vary with adherence and program quality. Weight management remains pivotal; lifestyle change, nutrition support, and, when appropriate, anti-obesity medications or metabolic surgery can reduce OSA severity by addressing the root driver of airway collapsibility. Not everyone achieves remission with weight loss alone, but even partial improvement can make other therapies more comfortable and effective.
Data is the quiet revolution. Modern PAP systems can adjust pressures breath-by-breath and transmit usage and leak metrics for remote coaching. Oral appliance titration increasingly draws on home sleep tests and wearable surrogates to iteratively find the sweet spot. Clinicians are exploring models that predict who will succeed with each modality by factoring in craniofacial structure, loop gain (a measure of ventilatory control), arousal threshold, and muscle responsiveness. Emerging pharmacologic research targets these traits—aiming, for example, to stabilize breathing control or reduce arousal propensity—though most candidates are still investigational and not yet routine care.
Expect continued convergence: smarter sensors guiding therapy in real time, 3D-printed custom appliances, and telehealth programs that blend education, troubleshooting, and behavioral support. The promise is not a single miracle device, but a toolkit that adapts as people’s bodies and lives change, making long-term success more attainable and less burdensome.
Living With Treatment: Practical Tips, Lasting Results, and What Comes Next
Success with sleep apnea therapy is part equipment, part habit, and part mindset. Early weeks matter: small wins build comfort and momentum. For PAP users, a professional mask fitting can prevent months of frustration. Begin with short practice sessions while awake, add humidification to ease nasal dryness, and experiment with ramp settings that start low and rise gently. Keep straps snug but not tight, and prioritize nasal health with saline rinses if congestion is an issue. Clean equipment regularly and replace consumables on schedule to maintain hygiene and seal integrity.
Simple habits amplify results:
– Keep a consistent sleep–wake schedule to stabilize circadian rhythms
– Avoid alcohol near bedtime and discuss sedatives with a clinician
– Sleep on your side if events are position-dependent
– Elevate the head of the bed to reduce airway collapse and reflux
– Maintain regular physical activity to support weight and metabolic health
For oral appliance users, follow-up is essential. Jaw discomfort often eases with gradual advancement; if dental changes arise, early adjustment can protect bite alignment. Pairing the device with positional strategies or nasal optimization may enhance effect. After any treatment change, a repeat sleep study—often at home—verifies that progress on paper aligns with how you feel during the day.
When should you seek re-evaluation? Consider it if sleepiness returns, snoring rebounds, weight shifts significantly, or new medical conditions emerge. People with resistant hypertension, recurrent atrial arrhythmias, or heart failure symptoms should ensure their sleep-disordered breathing is fully assessed and treated. If pregnancy is on the horizon, discuss sleep health early; addressing snoring and breathing disturbances can support maternal well-being and safer rest.
Conclusion: The landscape of sleep apnea care is moving from rigid protocols to responsive, person-centered plans. Established therapies are more comfortable and connected than ever, while newer options widen the path to relief for those who struggled before. Your role is to choose a sustainable starting point, track how you feel, and partner with a knowledgeable clinician who can tune the plan as life evolves. Night after night, better breathing reshapes days—steadily, measurably, and in a way that aligns with your goals and routines.


