Migraine Relief: Practical, Evidence-Based Ways to Ease Symptoms
Outline and Why Migraine Relief Matters
Migraine affects roughly one in seven people worldwide and ranks among the top causes of disability for adults under 50, especially women. Beyond pain, it drains attention, workdays, and social plans, often arriving with nausea, light sensitivity, and brain fog. The good news is that predictable patterns create leverage: when you know the phases, triggers, and decision points, migraines become more manageable. This article blends research with practical tactics you can use immediately and over time. To set expectations and provide a roadmap, here is the structure we’ll follow, followed by an in-depth dive into each part.
– Section 1: Outline and Why Migraine Relief Matters — the map you can keep on your desk.
– Section 2: Migraine 101 — how attacks unfold, what symptoms mean, and when to seek urgent care.
– Section 3: Acute Relief You Can Use Today — stepwise actions during an attack, from environment tweaks to medicines.
– Section 4: Prevention and Lifestyle — building a routine that steadies the nervous system and reduces attack frequency.
– Section 5: Conclusion and Practical Plan — turning knowledge into a weekly playbook tailored to your life.
Why relief strategies need both speed and patience: migraine is a neurological condition with waves. Acute tactics aim to shorten a current attack; prevention aims to reduce the number and intensity of future waves. The most successful plans combine both. Consider two contrasting scenarios. In the first, an attack catches you late, after dehydration and missed meals; medication works slowly and the day is lost. In the second, early signs cue water, food, a dark room, and timely medication; the arc bends shorter and milder. Our goal is to make the second scenario more common by clarifying what to do and when to do it.
Evidence highlights a few themes worth keeping in mind: early treatment improves outcomes; consistency in sleep, hydration, and meals lowers attack likelihood; and personalized plans trump one-size-fits-all. As you read, note strategies that fit your patterns. You do not need perfection—just enough consistency to tilt probabilities in your favor. Think of this guide as a toolkit: pick up the tool you need today, and steadily arrange the rest within reach for tomorrow.
Migraine 101: What’s Happening, and Why It Matters
Migraine is not “just a headache.” It is a brain-state shift involving the trigeminovascular system, neuropeptides such as CGRP, and sensory processing changes that heighten sensitivity to light, sound, and movement. Attacks often progress through phases: a premonitory period (hours to a day of yawning, neck stiffness, food cravings, mood changes), possible aura (visual or sensory disturbances in about a quarter of people), the headache phase (4–72 hours, sometimes moderate to severe), and a postdrome (“migraine hangover”). Recognizing your phases is powerful because it enables earlier, more targeted action.
Common features include:
– Throbbing or pressure-like pain, often one-sided but not always.
– Photophobia and phonophobia, which together strongly suggest migraine rather than tension-type headache.
– Nausea and sometimes vomiting, reported by a majority of people during attacks.
– Worsening with routine physical activity, such as climbing stairs.
Aura deserves special mention. Visual aura often appears as shimmering zigzags or blind spots evolving over 5–60 minutes, sometimes followed by sensory changes like tingling. Aura is typically reversible and fully resolves. Importantly, aura without headache can occur. The distinction between aura and warning signs of emergencies matters. Sudden “thunderclap” onset, the worst headache of your life, new neurological deficits (e.g., weakness, persistent speech difficulty), a stiff neck with fever, or new-onset headache after age 50 warrant urgent medical evaluation.
Triggers are not causes, but they can load the dice. Frequent contributors include sleep disruption, dehydration, skipped meals, stress spikes and letdowns, hormonal shifts, bright or flickering light, certain odors, and rapid weather changes. Some foods act as triggers for specific individuals rather than universally. A headache diary helps identify your patterns by tracking date, sleep, hydration, meals, stress, exposure to triggers, and response to treatment. Over a few weeks, trends emerge—perhaps late dinners plus evening screens predict next-day attacks, or perhaps long-cardio days are protective. Data from your own life is often the most actionable evidence you’ll ever gather.
Finally, consider the concept of allostatic load—the cumulative strain from stress, irregular routines, and environmental noise on a sensitive nervous system. Reducing load by smoothing daily rhythms is a cornerstone of prevention. When you see migraine through this lens, relief becomes not only an emergency response but a daily practice of keeping the system steady.
Acute Relief You Can Use Today: Shortening the Current Attack
When an attack begins, minutes matter. Early intervention—ideally at pain onset or during premonitory signs—consistently improves outcomes compared with waiting until pain is severe. Begin with environment and physiology while you prepare your medical options. Darken the room, reduce noise, and avoid strong smells. Hydrate with water or an electrolyte drink; pair fluids with a small, protein-containing snack if you have not eaten. Apply a cool pack to the forehead or neck, and consider brief paced breathing (for example, inhale 4 seconds, exhale 6–8 seconds) to ease sympathetic arousal that can amplify pain perception.
Medication choices fall into broad categories.
– General analgesics: anti-inflammatories and acetaminophen help many, especially when taken early and at adequate doses.
– Migraine-specific agents: triptans target serotonin receptors to block pain pathways; newer options like gepants (CGRP receptor antagonists) and ditans offer alternatives when triptans are not suitable.
– Antiemetics: for nausea and gastric stasis that can delay drug absorption; these agents can be helpful as add-ons.
Comparisons can guide choice. General analgesics are widely accessible and can be effective for mild-to-moderate attacks, but they may fall short for severe attacks or when nausea hampers absorption. Triptans often act faster and more completely when taken early, but they are not appropriate for some cardiovascular conditions. Gepants and ditans can be used when triptans are contraindicated or poorly tolerated; they may have different side-effect profiles and do not cause vasoconstriction. Discuss options and contraindications with a clinician to match your health history and attack pattern.
Practical rules of thumb help avoid pitfalls.
– Treat early and do not redose repeatedly without guidance; overuse can lead to more frequent headaches.
– As a rough ceiling, limit acute medication days to 2–3 per week on average to reduce the risk of medication-overuse headache.
– Consider non-oral formulations (nasal, injectable, orally disintegrating) when nausea or rapid escalation is typical.
– Caffeine can enhance analgesics for some, but excessive daily intake or abrupt withdrawal can backfire; aim for a consistent routine rather than spikes.
Neuromodulation devices (external nerve stimulation) and non-drug methods like gentle neck mobility, progressive muscle relaxation, or mindfulness can complement medication. While evidence quality varies by method, low-risk options are reasonable to try, especially when you log results. An example stepwise plan: at first sign, hydrate and darken the room; take your chosen acute medication; lie down with a cool pack and practice 5 minutes of slow breathing; reassess at 60–90 minutes per your medication’s instructions. If inadequate, follow your clinician’s rescue plan. Keep tools packaged together in a “migraine kit” so decisions are easier when you are not at your sharpest.
Prevention and Lifestyle: Lowering the Odds Before the Storm
Prevention is about tilting probabilities. Because migraine is a condition of heightened sensory and stress reactivity, the nervous system thrives on rhythm. Three pillars—sleep, nutrition and hydration, and movement—anchor most prevention plans, with supplements and trigger management filling the gaps. A consistent routine may sound mundane, but studies repeatedly link regularity with fewer monthly migraine days.
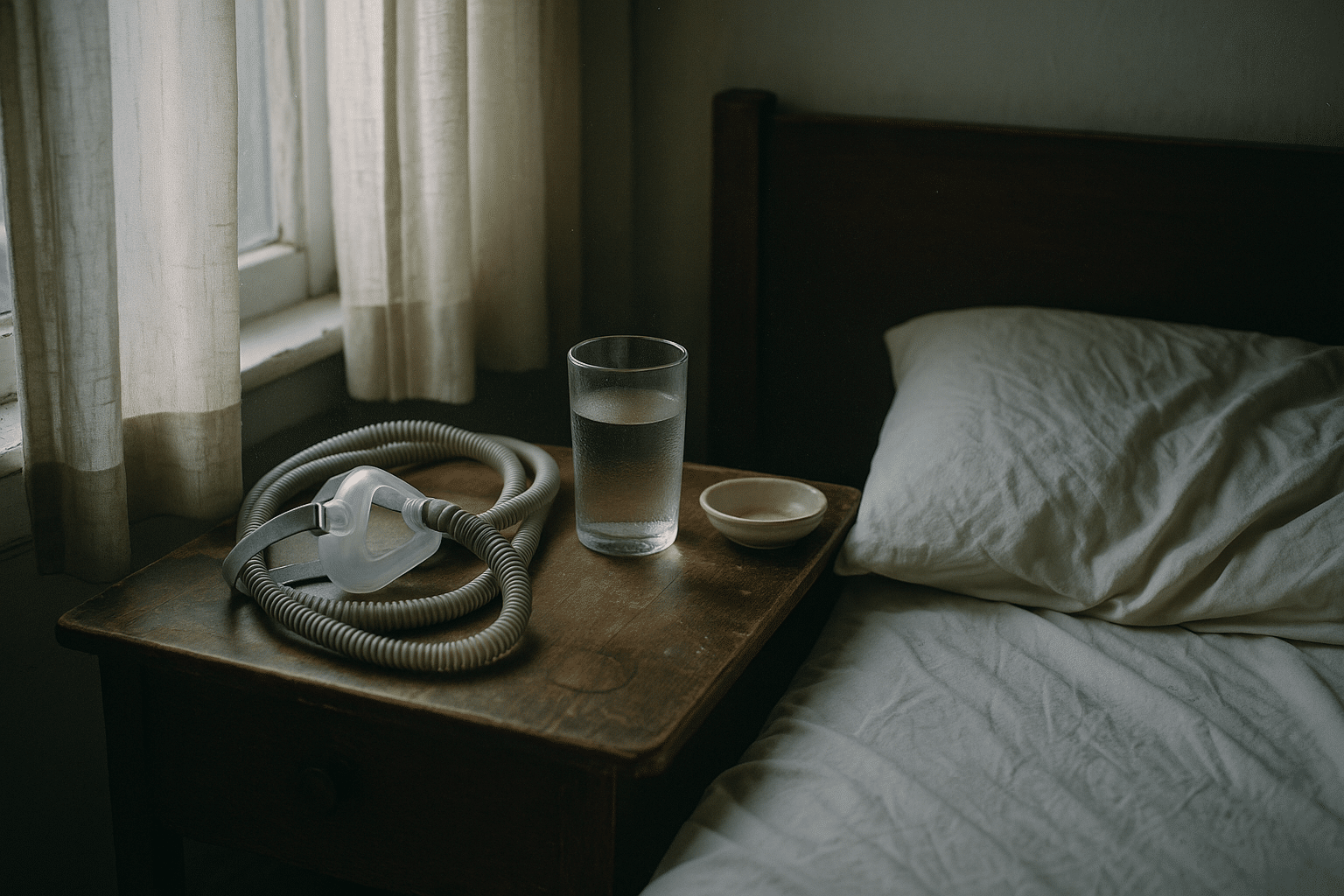
Sleep: Aim for a stable sleep-wake schedule, even on weekends. Both sleep loss and oversleeping can precipitate attacks, so think “regular,” not “more.” Optimize sleep hygiene: a dark, cool bedroom; wind-down time without screens; and a consistent wake-up. If snoring, gasping, or unrefreshing sleep is common, discuss evaluation for sleep apnea, which can exacerbate headaches.
Nutrition and hydration: Skipped meals are a well-known trigger, likely via glucose and hormone fluctuations. Eat balanced meals on a schedule—include protein and fiber to blunt spikes and crashes. Hydration targets vary by body size and climate; as a simple nudge, carry a water bottle and check that your urine is pale yellow. Caffeine consistency matters; choose a daily window and dose, and avoid late-afternoon intake that sabotages sleep.
Movement: Aerobic exercise 3–5 days per week has been associated with fewer attacks in several studies. Start modestly and progress gradually, since intense, abrupt exertion can provoke headaches in some. Compare approaches:
– Aerobic sessions (e.g., brisk walks, swimming) improve cardiovascular fitness and mood.
– Gentle strength training enhances posture and neck/shoulder stability that may reduce musculoskeletal contributors.
– Yoga and mobility work reduce stress reactivity and muscle tension; randomized trials suggest meaningful benefits for frequency and intensity in some participants.
Supplements: Evidence supports a few options as part of a comprehensive plan. Magnesium (often 400–600 mg elemental per day, forms like citrate or glycinate) may help reduce frequency and is generally well tolerated; loose stools can occur. Riboflavin (vitamin B2, 400 mg/day) and coenzyme Q10 (100–300 mg/day) have supportive, though variable, evidence. Discuss with a clinician, particularly if you are pregnant, breastfeeding, or have kidney issues. Some herbal products have safety concerns; for example, certain butterbur preparations can be hepatotoxic unless rigorously purified.
Trigger management and stress skills: You cannot avoid every trigger, but you can reduce the cumulative load. Identify high-yield modifications: earlier bedtime, a morning light walk, prepared snacks to prevent meal gaps, screen breaks for eyes and neck, and boundary-setting around noisy environments when feasible. Simple techniques—brief diaphragmatic breathing, a 60-second body scan, or a short stretch routine—can shift physiology away from fight-or-flight. Importantly, prevention is cumulative. A few small habits, repeated most days, often outperform sporadic big efforts.
Conclusion: Your Practical Plan for Calmer, Shorter Attacks
Personalizing care turns scattered advice into traction. If you experience four or more migraine days per month, or if attacks are particularly disabling, talk with a clinician about preventive medications. Options include beta-blockers, certain antiepileptics, tricyclic antidepressants, CGRP-targeting treatments, and, for chronic migraine, botulinum toxin type A injections administered by trained professionals. Short-term “mini-prevention” around predictable triggers (for example, perimenstrual periods) can be considered. Choice depends on your medical history, potential side effects, and preferences. Meanwhile, non-drug foundations still matter; they can boost the effectiveness of any prescription plan.
Build your weekly playbook by combining actions across time horizons.
– Daily: regular sleep and meals, hydration, brief movement, and a few stress resets.
– Weekly: two to three aerobic sessions, one or two strength or yoga sessions, and a review of your headache diary to spot patterns.
– Attack plan: a ready-to-use kit with fluids, a cool pack, a mask for light sensitivity, and your agreed acute medication with clear timing instructions.
Special cases deserve added nuance. Hormonal migraine may respond to steady routines, magnesium, and preventive options discussed with a clinician; some benefit from short-term preventive strategies timed to cycles. During pregnancy and breastfeeding, the safety profile of medications changes; professional guidance is essential. People with cardiovascular disease, uncontrolled high blood pressure, or complicated aura need tailored choices. Red flags such as a thunderclap onset, new neurological deficits, fever with stiff neck, head trauma, or a rapidly worsening pattern call for urgent evaluation rather than home management.
Work, school, and travel can be more manageable with simple accommodations. Keep a water bottle at your desk, adjust screen brightness, use blue-light filters if helpful, schedule short breaks, and stash a small “migraine kit” in your bag. When traveling, preserve sleep and meal timing as much as possible; pack earplugs and an eye mask, and plan for hydration in dry cabins or climates.
Here is a concise starting blueprint you can adapt this week:
– Mornings: brief outdoor light exposure, hydrate, and eat breakfast within an hour of waking.
– Midday: 10-minute walk, water refill, and a protein-rich snack.
– Evenings: a defined caffeine cutoff, screen dimming, and a 30-minute wind-down before bed.
– At first signs of attack: fluids, dark room, cool pack, and your chosen acute medication early, then reassess per instructions.
Relief rarely arrives as a single breakthrough; it shows up as a series of small, steady wins. With a clear plan, early action, and a willingness to refine based on your own data, you can shorten attacks, reduce their frequency, and reclaim more predictable days. Keep the toolkit handy, review what works, and let consistency do the quiet, transformative work over time.